Categories
Hysteroscopic Surgery: What It Is, When It’s Needed, and What Recovery Looks Like
Jun 23, 2025
When you hear the words hysteroscopic surgery, it may not be the procedure itself that worries you, but the silence around it. There’s often too little said. Or too much, too quickly. Either way, it leaves you confused. What is it, really? Is it painful? Will it affect your chances of having a child? And how long until you feel like yourself again? At BirthRight by Rainbow Hospitals, we don’t believe in rushing past these questions. We believe in answering them with calm, clarity, and respect. This guide is meant to do just that, quiet the noise, and help you understand what this procedure means for you.
What Is Hysteroscopic Surgery?
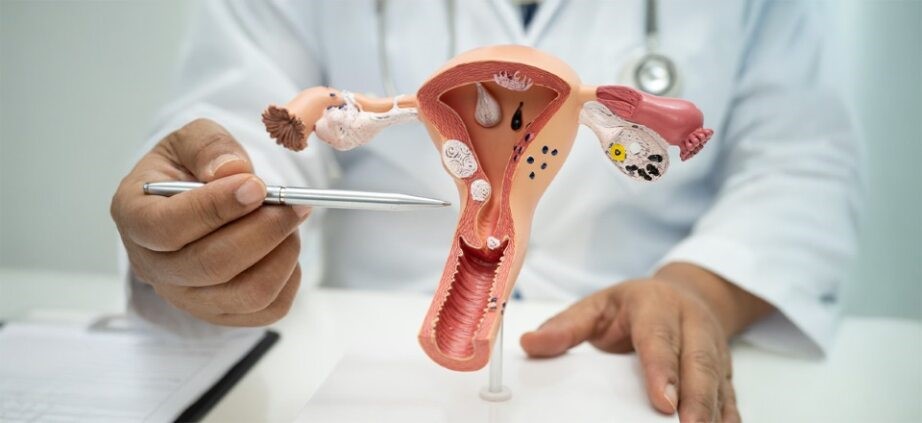
It’s simple. And precise. Hysteroscopic surgery is a way for your doctor to look inside your uterus without making any cuts. A small, lighted tube, a hysteroscope, is passed through your vagina and cervix. It gives a clear view of the uterine cavity. If something needs to be treated, fibroids, polyps, retained tissue, it can be done right then and there. No stitches. No hospital stay. Just clear access to a part of your body that often stays hidden.Common reasons for hysteroscopic surgery include:
- Removing fibroids or polyps
- Investigating heavy or irregular bleeding
- Diagnosing infertility or repeated miscarriages
- Treating adhesions (Asherman’s Syndrome)
- Correcting structural issues like a uterine septum
- Removing retained tissue after miscarriage or delivery
What To Expect After Hysteroscopic Surgery?
Knowing what to expect is a form of healing. It allows you to stop imagining the worst and focus on what’s real.Right After the Procedure
There might be some cramping. Light bleeding. Maybe a little dizziness, especially if you’ve had anesthesia. These are temporary. They pass in a day or two. You’ll be awake. You’ll go home the same day. You’ll walk out with more clarity than you walked in with.Physical Recovery
Most women return to their routine within 1–2 days. But routine doesn’t mean rush. Let your body close the door slowly. Here’s what helps:- No heavy lifting for a few days
- No sexual activity until your doctor says it’s okay
- Rest. Hydrate. Eat simply.
Emotional Recovery
Sometimes, the body recovers faster than the mind. If this procedure was tied to fertility, miscarriage, or chronic symptoms, you may carry more than just physical tension. That’s normal. You’re not being “too emotional.” You’re being honest. If you need to talk, talk. At BirthRight by Rainbow Hospitals, you’ll find someone who listens. Not with checklists. But with presence.Follow-Up
Your doctor will likely ask you to return in a week or two. If tissue was sent for testing, this is when results are shared. Healing is checked. Call earlier if you notice:- Strong pain
- Heavy bleeding
- Unusual discharge
- Fever or chills
When Does Hysteroscopic Surgery and Laparoscopic Ovarian Cystectomy Work Together?
Sometimes, one view is not enough. While hysteroscopy looks inside the uterus, laparoscopic ovarian cystectomy looks outside, at the ovaries and surrounding structures. When done together, the care is complete. One procedure addresses what’s happening inside the uterus; the other, what’s happening around it. A laparoscopic ovarian cystectomy may be recommended if you have:- Ovarian cysts
- Endometriosis
- Adhesions in the pelvis
- Symptoms not explained by uterine issues alone